Essential Hydration & Electrolyte Tips for Cancer Treatment – Beat Vomiting & Stay Strong
By Mark Brown, RN | Oncology Nurse & Co-Founder of Dermavitality
Why Does Cancer Treatment Cause Nausea?
Cancer treatments like chemotherapy and radiation can quickly dehydrate your body, especially when nausea or vomiting comes into play. Dehydration isn’t just uncomfortable — it can worsen fatigue, impact kidney and skin health, and compromise how well your treatment works.
Hi, I’m Mark Brown, RN—an oncology nurse who’s seen how effective simple hydration and electrolyte strategies can be in keeping patients stronger and more comfortable. In this post, we’ll explore nurse-approved methods, backed by cancer center guidance and clinical research, to help you stay hydrated, manage electrolytes, and soothe your body during treatment. Keep reading to find out how to sip, restore, and protect your body every day.


Why Hydration and Electrolytes Matter?
Chemotherapy and radiation can cause rapid fluid loss through vomiting, diarrhea, fever, excessive urination, or even medication side effects mdanderson.org. When fluid and electrolytes like sodium, potassium, and magnesium drop, symptoms escalate: headaches, muscle cramps, low blood pressure, kidney stress, and increased fatigue .
Doctors often prescribe oral rehydration solutions (ORS)—balanced blends of water, sugar, and electrolytes—to address moderate dehydration Healthline.com. If hydration is not possible by mouth, intravenous fluids may be necessary healthline.com.com+10. Keeping these levels stable isn’t just comfortable—it’s essential for safe treatment and recovery.
How Cancer Treatment Triggers Dehydration?
Chemotherapy works by targeting rapidly dividing cells, which unfortunately includes the cells lining your stomach and intestines. When these cells get damaged, you may experience inflammation and delayed digestion—leading to nausea, bloating, and diarrhea.
At the same time, chemo and radiation affecting the chemoreceptor trigger zone (CTZ) in your brain can cause nausea—even with an empty stomach. Radiation to the abdomen, pelvis, or brain amplifies these symptoms by further disrupting normal gut and neurological function mdanderson.org.
When nausea or vomiting strikes, fluid and vital electrolytes are lost quickly, making swift replenishment critical to keep you safe and energized.

Spotting Dehydration - Know the Signs
Falling behind on hydration can worsen quickly. Watch out for:
If you notice these symptoms—or can’t drink fluids for over 24 hours—it’s time to contact your healthcare team.
Severe dehydration may require IV fluids or prescription ORS.

Nurse Tips for Hydration & Electrolyte Recovery
Sip Small & Often
- Drink 5–10 oz of liquid every 30 minutes through the day. Keeps intake steady and prevents overwhelm.
- Try water, clear broths, herbal teas, or ORS 10 Foods that may help cancer patients stay hydrated.
- Carry a refillable water bottle—set reminders if needed.
ADD ELECTROLYTES
- Use ORS mixes like Pedialyte or Citrate-based solutions that balance sodium and potassium.
- If unavailable, mix 1 liter water + ½ tsp salt + 2 Tbls sugar + a squeeze of lemon to gently rehydrate
- Useful articles:
How to Stop Throwing Up and Avoid Dehydration
How Oral Solutions Help to Manage Dehydration
AFTER VOMITING
- Wait 5–10 minutes before sipping again
- Begin with small sips; once stable, move to clear fluids, then bland foods.
Avoid Sugary Sports Drinks
- Limit to small portions—many contain too much sugar or artificial dyes
- Opt for simple ORS, water-rich soups, or fresh juices.
- What is ORS: Water, Salt (sodium chloride) Sugar (usually glucose) It's designed to quickly restore fluids and electrolytes lost due to vomiting, diarrhea, or dehydration—common during cancer treatment.

Why ORS Matters for Cancer Patients:
- When patients can’t keep food or water down, ORS helps prevent serious dehydrationand electrolyte imbalances without needing IV fluids.
- It's used worldwide and recommended by major institutions like the World Health Organization (WHO), CDC, and MD Anderson for safe, at-home hydration.
Homemade ORS Recipe (WHO-recommended):
HOMEMADE ORS (1 LITER RECIPE)
Try the BRAT
Diet After Vomiting If you're recovering from vomiting or nausea, the BRAT diet can help ease your stomach back into eating. BRAT stands for:
These foods are bland, low in fiber, and gentle on the digestive system. They're easy to digest and unlikely to trigger further nausea. You can also add in clear broths, saltine crackers, or plain oatmeal as tolerated.
Start slow: Take small bites, chew well, and wait 15–20 minutes between foods. Once you’re stable, gradually reintroduce protein and other nutrient-dense options.
- Keep a hydration log noting fluid types and amounts.
Track Fluid Intake

- Urine color is also a useful indicator—aim for pale straw.
Know When IV Fluids Are Needed
- Persistent vomiting or diarrhea, or critical symptoms like confusion or heart irregularity require immediate medical attention. Remember if you are having problems withkeeping fluids down call your nurse or doctor. A bag or 2 of IV fluids can help you feel better and make a huge difference. It is better to be proactive and call to get some hydration than to end up in the emergency room in a hrisis. Don't hesitate to call youcare team and get some IV hydration if you are not feeling well.
- Useful articles.
Dehydration and Lack of Fluids American Cancer Society


Electrolytes Explained—Why They Matter
- Sodium regulates blood volume and pressure.
- Potassium supports muscle and nerve function.
- Magnesium helps with energy, cramps, and nerve health.
Cancer therapy can deplete these nutrients. Oral rehydration first helps restore balance,but in high-risk regimens like cisplatin-based chemo, the hydration protocols include pre-and post-treatment IV saline to protect the kidneys.
In rare complications like tumor lysis syndrome, your fluid and electrolyte needs maybecome especially tricky—make sure your care team knows you’re vomiting or havingdiarrhea.
Special Strategy for Vomiting Patients
- Stick to ORS; slow sips after vomiting are key .
- Offer cold popsicles from ORS or diluted broth for easy intak
- Ginger tea and deep breathing techniques may help settle nausea
- Call your provider if vomiting prevents all fluid intake for over 24 hours.
- Useful articles.
Dehydration: Giving Liquids at Home

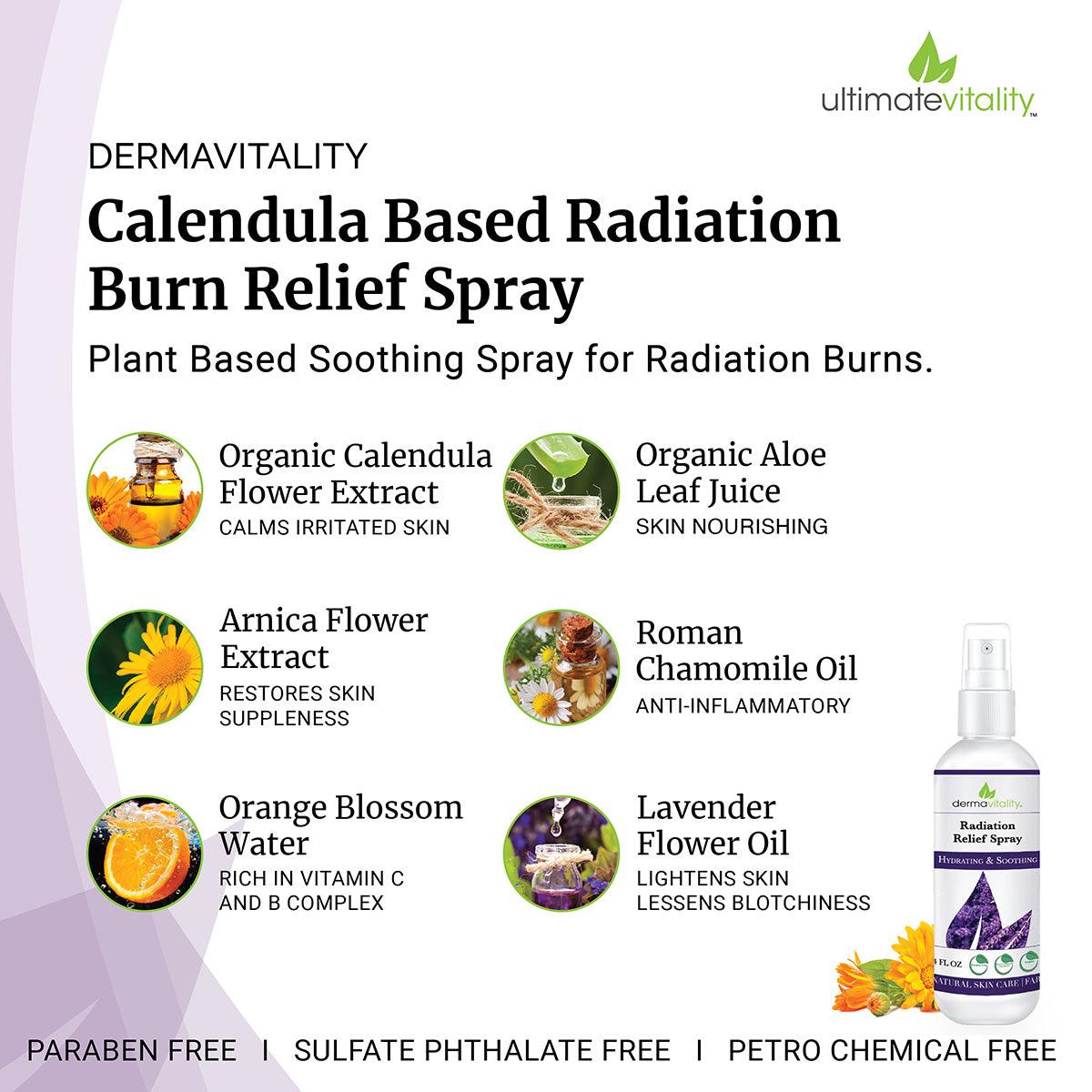
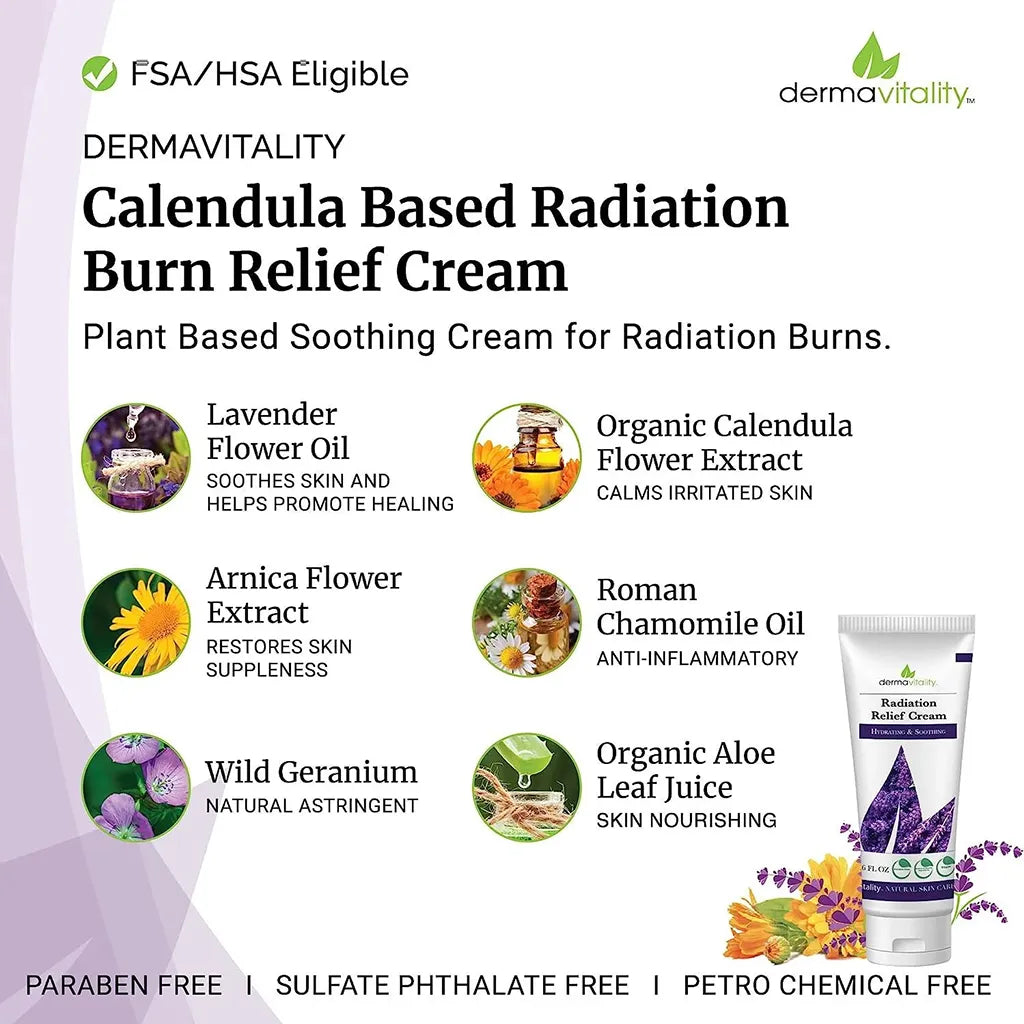
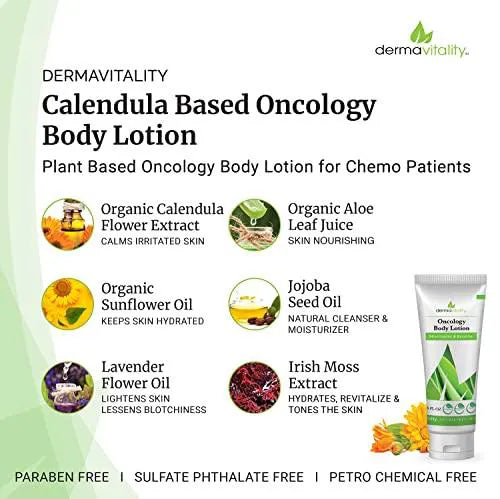
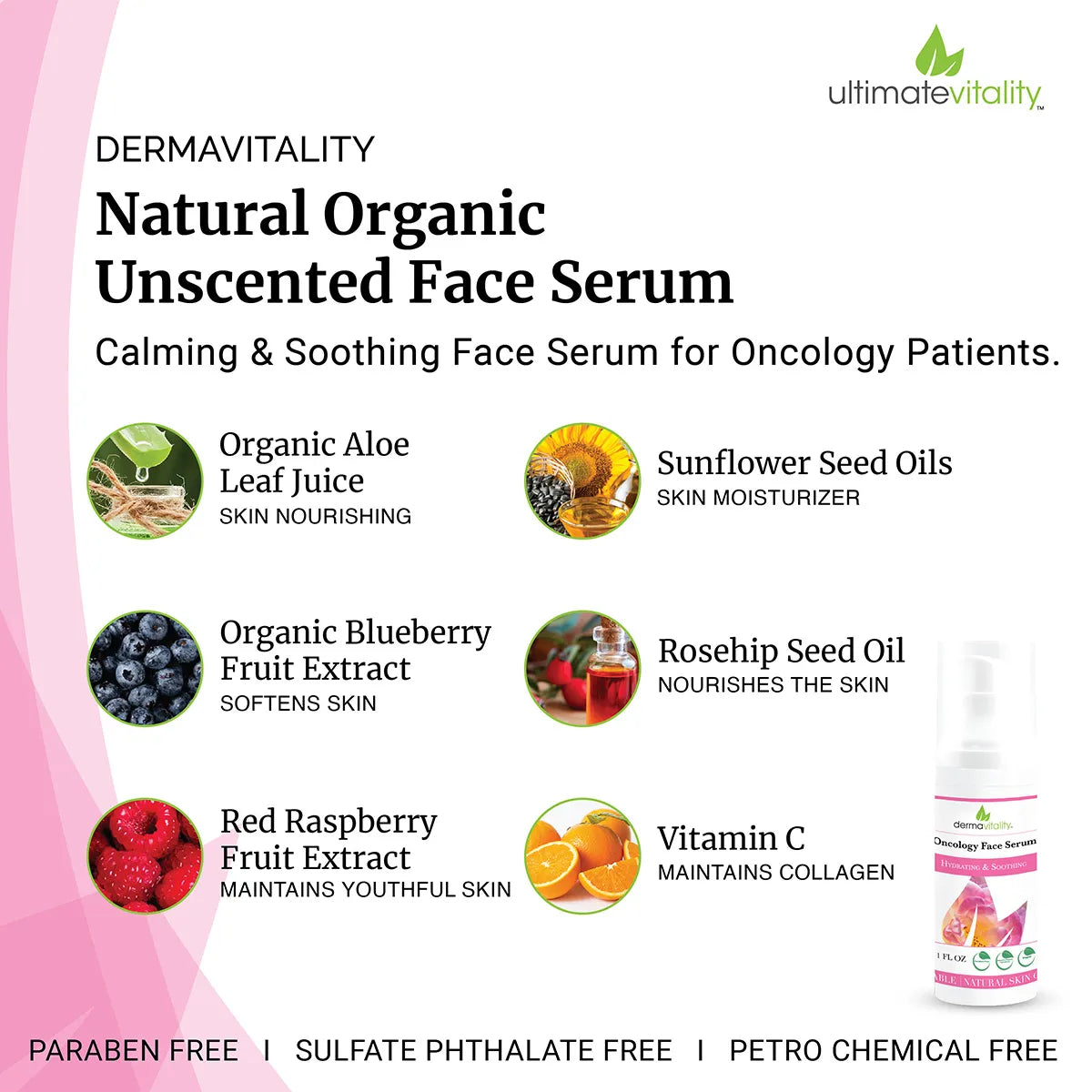
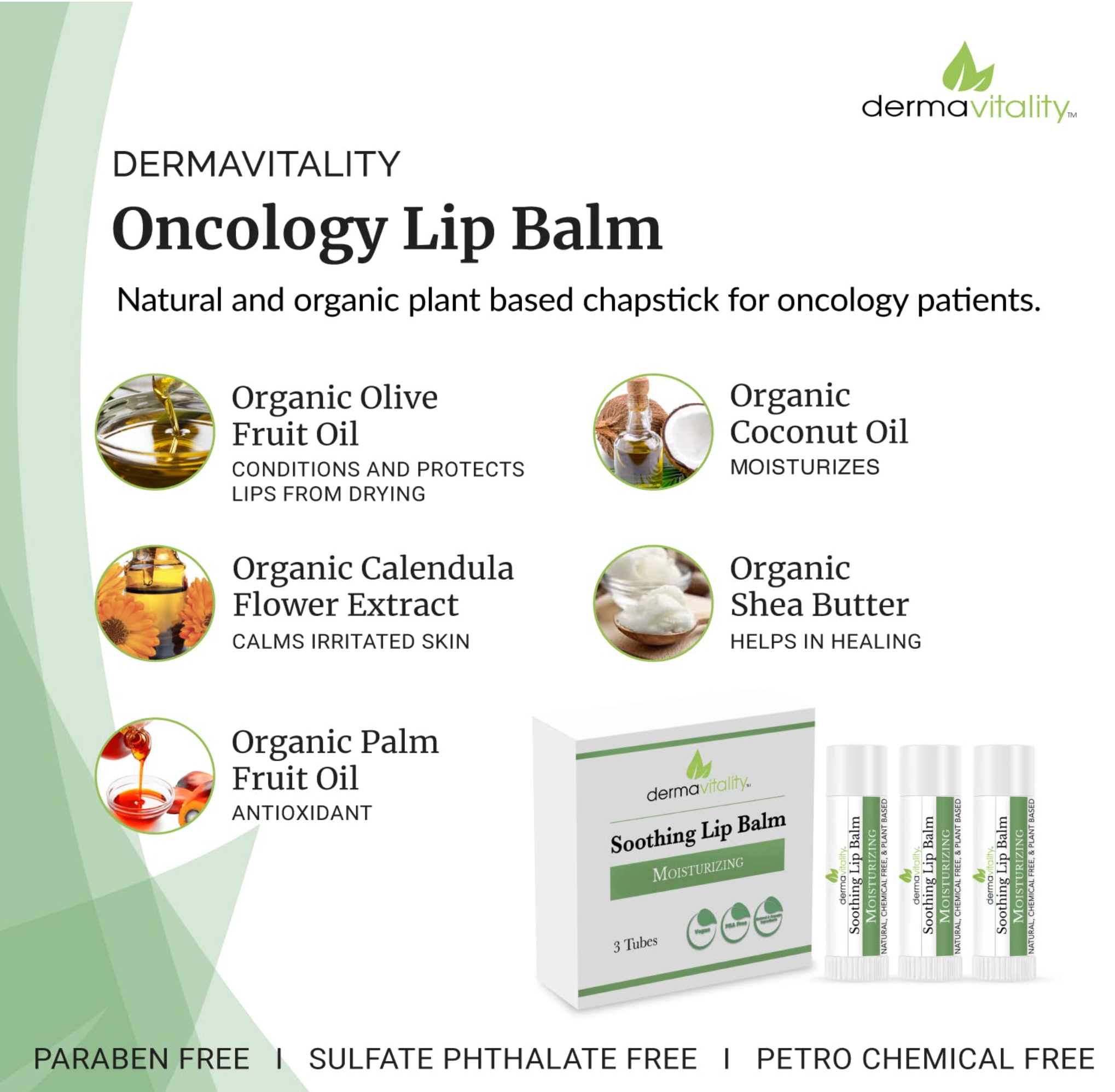
Nutritional & Skin Care Connections
Stay hydrated and nourished, and your skin absorbs it too. Studies show proper hydration supports skin integrity and reduces treatment-related dryness Include fluid-rich foods like soups, smoothies, watermelon, cucumber and celery to support both hydration and nutrition. Pair electrolytes with proteins like bone broth or yogurt to help rebuild strength.

When It’s Time to Call Your Care Team
- No fluid intake or urine output for 24 hours
- Confusion, fainting, fast heartbeat
- Blood in vomit or stool
- Severe electrolyte imbalances or kidney concerns
- Early intervention may include IV fluids, electrolyte monitoring, oradjustments to your treatment plan.
Final Thoughts from Nurse Mark
You’re doing fantastic. Every sip and small step toward hydration helps your body and mind feel stronger. Consistency—tiny, frequent efforts—are better than forcing big volumes.
Trust your body signals, lean on your care team, and know that managing hydration is one of the most powerful things you can do for your healing journey.

Disclaimer
The information provided here is for educational purposes only and is not a substitute for professional medical advice. Always consult your physician, advanced practice nurse, or qualified healthcare provider with questions about your condition or treatment.